
The bilharziosis parasites (schistosoma) are sanguinary, minute flat worms to be found in great quantities in blood vessels of the abdomen. Five of the species are pathogenic for humans. The initial clinical manifestations of the disease which they give rise to, Schistosomiasis, are either cystic or intestinal. Other organs are invaded by the eggs of these worms, the liver and the spleen being privileged targets.
Known since very ancient times and widespread in the tropics, where it affects some 300 million individuals, Schistosomiasis figures among the most virulent epidemics in sub-Saharan Africa, the West Indies and South East Asia.
Right from the beginning of colonization, physicians make the first epidemiological inquiries. And then, in the service of the AMI, as the years go by, millions of patients are detected and treated. Only derivatives of Antimony prove to be somewhat efficacious. It is only in 1975, after decolonization, that the first really efficacious medicine, Niridazole, arrives.
The Colonial health service distinguishes itself, on the one hand, in descriptions of radiological signs of cystic Schistosomiasis; on the other hand, in the study of large spleens and livers due to the disease; finally, in surgical methods for dealing with complications.
The collective prophylaxis of these diseases depends on urinary and faecal hygiene, the combat against the pollution of dams, rivers and backwaters and the destruction of molluscs (water snails), intermediary hosts of the embryos eliminated with the faeces and urine of the patients.
SCHISTOSOMA THAT ARE PATHOGENIC FOR HUMANS AND THEIR BIOLOGY
– Urinary bilharziosis, essentially cystic, is due to a schistosoma called Schistosoma haematobium whose eggs, passing through the mucous membrane of the bladder, are eliminated together with urine. The principle symptom is the periodic presence of blood at the end of micturition.
– Intestinal bilharziosis is due to four other species (Schistosoma mansoni, Schistosoma intercalatum, Schistosoma japonicum, Schistosoma mekongi). In each case, the eggs, going through the mucous membrane of the rectum, are eliminated with the faeces. Repeated diarrhoea is a sign of the disease but remains often unperceived.

Carried by flowing water towards ponds and wells, these eggs hatch out in a few minutes to a moving embryo. It only survives if it encounters a fresh water snail (a particular snail for each species) and penetrates it. Within the organism of this mollusc, it undergoes a series of transformations. A few weeks later, "contaminating larvae" leave the mollusc and spread over the surrounding waters. By pricking, they pass actively through the skins of bathers or of those who are simply crossing the backwater. In fact, contamination is generally contracted in childhood (between the ages of 6 and 10 years).
After a series of transformations, adult worms, entrenched in vessels deep down in the abdomen, are doted with formidable longevity : for about twenty years, the females lay an impressive number of eggs, most of which are eliminated outside the body, except those which, transported by blood, are going to cause troubles in the genitor-urinary apparatus, the liver, the spleen and the lungs.
In endemic zones, the great majority of the population is infected but remain apparently "in good health" all their lives, except for some occasional and brief periods of diarrhoea and the emission of bloody urine.

THE FIRST EPIDEMIOLOGICAL INVESTIGATIONS
Urinary bilharziosis is a disease that is essentially African. Since the "blood pissing" of Saharan caravaneers of the 14th Century, native populations have known the symptoms. As early as 1749, the French explorer Adanson reports the presence in Senegal of the mollusc that is the intermediary host of the worm.

Frequent in Egypt (the presence of eggs in mummies), existing in North Africa, this "Schistosomiasis of the sands" is widespread in French West Africa (AOF). From 1912, Joyeux* reports its existence in Guinea, Bouet* and Roubaud* in Dahomey. In 1916, Clapier* finds 54 % of the population of a region in Guinea having the disease. Some investigations are limited to childhood, the age of predilection for contamination. According to M. Léger* and Redier*, if, in the city of Dakar, 6 % of the children are contaminated by the parasite, in the suburbs, the backwater zone, the rate of contamination is 39 %. One third of rural African populations are affected by this endemic.
In French East Africa (AEF), the distribution is less homogenous. Jamot*, Notais* and Robert* report it in Chad while, in 1920, it is thought that Oubangui and the Moyen-Congo are spared.
Studies show that, in Madagascar, the disease is present only in the western half of the island.
Urinary bilharziosis is unknown in Indochina and the West Indies.
Intestinal bilharziosis with Schistosoma mansoni is to be found especially in Brazil, Guyana, the West Indies and Black Africa. In Sudanese populations, Gaud* finds that the incidence of infection is between 60 and 80 %, figures that match those in Chad or Senegal. In Madagascar, the disease is confined to the south and the east (Raynal*, Brygoo*). It does not exist in Asia.
Bilharziosis with Schistosoma intercalatum is specific to Equatorial Africa. As for bilharziosis with Schistosoma japonicum, it engenders severe and acute forms. It is exclusively Asiatic with breeding grounds in Indochina.
It must be mentioned that the apparently capricious geographical distribution of schistosoma is a consequence of the way in which aquatic molluscs, the intermediary hosts of the parasites, are spread out.
X-RAY EVIDENCE OF URINARY SCHISTOSOMIASIS
The progress in x-ray technology and the arrival of the first radiologists of the Colonial Health Service result in interesting breakthroughs. In 1958, in Dakar, Pellegrino* shows the utility of x-rays of the lesser pelvis without preparation. After many years, the irritation caused by Schistosomiasis provokes thickening and calcification in the walls of the bladder, whose circumference becomes opaque to x-rays. When full, the bladder has the appearance of a regular globe whereas, after micturition, the same organ remains visible but all crumpled up like a deflated balloon. The Pellegrino* symptom is very useful in current practice...

Still concentrating on the domain of x-rays, the same scientist, using intravenous urography, describes with precision images of the urinary tract, profoundly deformed in the case of Schistosomiasis patients. Among other phenomena, the dilatation of cavities of the kidney result in images said to be "too beautiful", a sign of urethral stenosis.

LARGE LIVERS AND SPLEENS DUE TO SCHISTOSOMIASIS
Intestinal Schistosomiasis, essentially due to Schistosoma mansoni, provokes, at the end of fifteen or twenty years (therefore, in adults) a hypotrophy of the liver and/or the spleen.
On the clinical level, numerous colonial physicians contribute towards the study of these complications, among others F. Blanc*, M. Marin*, Charmot*, Armengaud*, Sankalé...
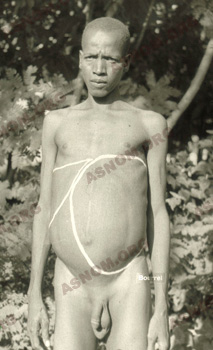

Splenomegaly due to bilharziosis: a drawing of the contour before ablation and the spleen after excision
Studying pieces of livers and spleens under the microscope, colonial anatomical pathologists contribute towards a better knowledge of these complications. In particular, Camain*, in Dakar, differentiates between lesions due to Schistosomiasis and those due to other tropical hepatic ailments. He describes the Schistosomiasis granuloma which leads, on the clinical level, to portal hypertension.
Finally, the threat of serious digestive haemorrhages or traumatic ruptures of certain giant spleens make colonial surgeons resort to interventions of which they codify the techniques and the indications.
SURGERY IN COMPLICATIONS OF SCHISTOSOMIASIS
During the whole of the colonial period, the medicinal treatment of Schistosomiasis being hardly efficient with repeated contaminations, the disease evolves in the same patient for many decades and a certain number of complications set in. Whether subject to sclerosis or calcification, old lesions remain irreversible and the recourse to surgery is a welcome palliative. Many surgeons of the Health Service distinguish themselves in this branch of surgery : Botreau-roussel*, Assali*, Dejou*, Delom*, Carayon*, Nosny*, Perquis*.
The principal indications for surgery are :
– In Urology, the contraction of the urethra and the spleen "destroyed", which justify ablation.
– In Gynaecology, chronic inflammations of ovaries and fallopian tubes, which cause sterility and extra-uterine pregnancies.
– In visceral surgery, anastomosis or vascular derivations in the course of certain complicated hepatomegaly due to digestive haemorrhage; or the ablation of the spleen which is awkward because of its volume.
– In Neurology, small tumours caused by Schistosomiasis which compress the brain or the spinal cord.
For further information :
– Deschiens R. : Les bilharzioses in Médecine Tropicale 2 vol. Par M. Vaucel p23-108. Editions médicales Flammarion. Paris 1954.
– Bull. OMS : Groupe de travail scientifique sur les bilharzioses. 1978.56,6,859-868.
– Camus D. Capron A. : Les bilharzioses. Presse Therm. Clim. 1979,116,2,72-91.
– Duflo B. Danis M. : Traitement et prophylaxie des bilharzioses. Bull. Soc. Path. Exo. 1981,75,575.
– Groupes d’auteurs : Numéro consacré aux bilharzioses. Rev. Prat. 1993,43,4,401-467.


